According to a recent DoD Inspector General report, thousands of active duty servicemembers and their families may have experienced delays in obtaining mental health care. The delays may have involved not being able to 1) see the right provider at the right time, 2) obtain mental health care at all, or 3) receive timely follow-up treatment.
These findings are consistent with anecdotal reports MOAA has received from active duty families and must be addressed to improve access to mental health care. MOAA is committed to leveraging these report findings to achieve improvements to mental health care access for servicemembers, retirees, their families, and survivors.
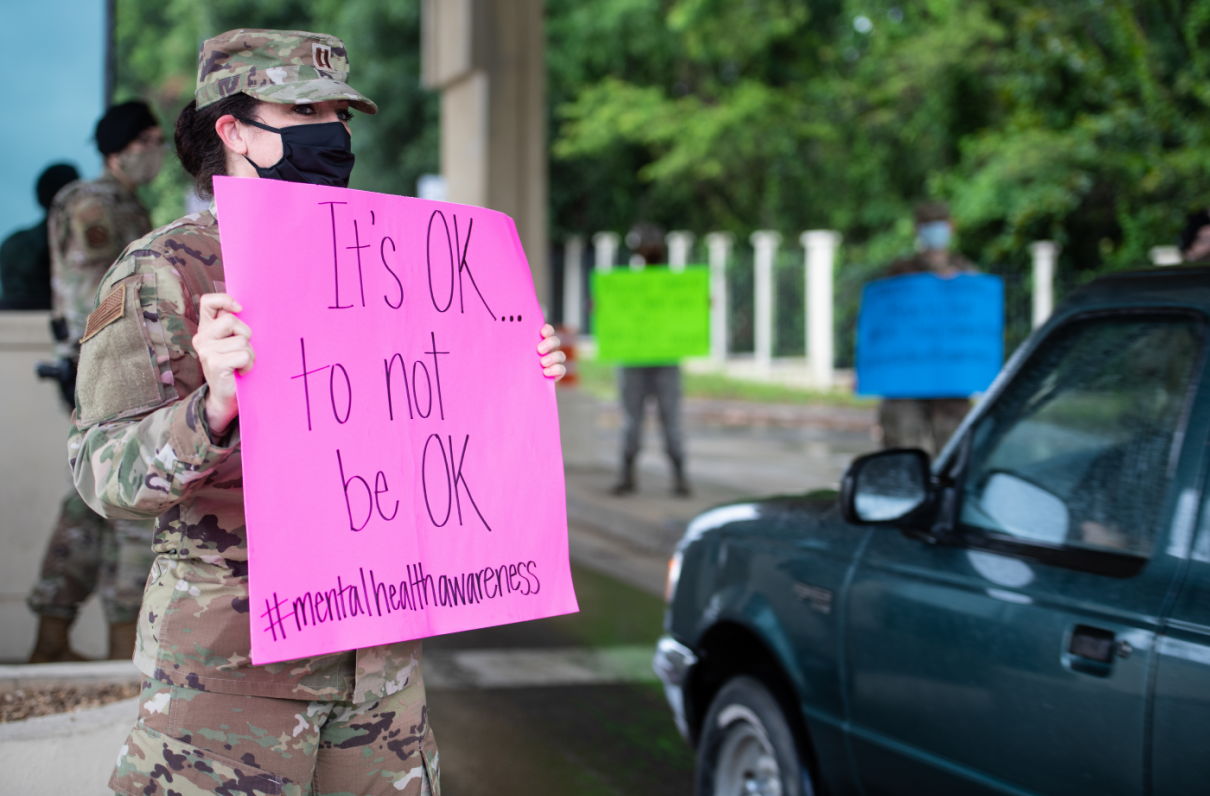
The combination of threats to the servicemember’s safety, lengthy family separations, frequent relocations, uncertainty, and lack of control can take a psychological toll on military families. Mental health is a critical part of every servicemember's medical readiness, the IG report states, and the well‑being of military families is critical to the readiness of active duty servicemembers. The report also notes DoD’s responsibility to effectively identify and treat mental health conditions through a consistent standard of care.
[RELATED: More Health Care Resources From MOAA]
The IG found DoD did not consistently meet outpatient mental health access-to-care standards. For the December 2018 to June 2019 reporting period:
- Seven of 13 military treatment facilities (MTFs) or their supporting TRICARE network did not meet the 28-day specialty mental health access-to-care standard in each month.
- An average of 53% of all active duty servicemembers and their families identified as needing mental health care and referred to the purchased care system did not receive care. In comparison, for all specialty care combined, 36% of patients referred to TRICARE civilian providers did not receive care.
TRICARE does not require a referral for mental health care, except for active duty servicemembers. The IG report did not evaluate access to care for those who self-refer to mental health care because the Military Health System (MHS) has no visibility or data on this population.
[RELATED: Attention, TRICARE Beneficiaries: Did One Appointment Trigger Two Copays?]
MOAA recognizes the challenges associated with a national shortage of many types of behavioral health providers, particularly those who treat children and adolescents. However, MOAA believes two of the IG report’s several recommendations have the potential to help military families access mental health care.
Ensuring Available Private-Sector Care
The report recommends the Defense Health Agency (DHA) “develop a method for the MHS to book patient appointments in the purchased care system to confirm patients are able to obtain care, except when a patient chooses to book directly with a purchased care provider.”
DHA agreed with the recommendation and stated a pilot program is being developed where beneficiaries will call MHS schedulers who will perform a “warm hand-off” to private-sector mental health providers and confirm availability of the required service within access-to-care standards. The DHA plans to make this voluntary; self-referred patients may use the appointing center to schedule a mental health appointment, but aren’t required to do so.
MOAA strongly supports this pilot. Not only will it assist beneficiaries with access to care, but it will allow DHA to document and track appointment availability within access standards for patients with referrals and those who self-refer and elect to use the MHS appointment booking system.
Report on Appointment Availability
TRICARE contractors submit a monthly network adequacy report to DHA, but the reports don’t include details on provider appointment availability. The IG report recommended adding this availability to the report, and DHA agreed, stating the next TRICARE managed care support contracts, scheduled to start health care delivery in 2023, will be updated to include such a requirement.
IG asked the DHA to provide a copy of the draft language of the next TRICARE contract requirements.
MOAA will follow up with DHA to discuss the possibility of directory accuracy requirements specific to behavioral health providers – this would eliminate duplicate listings, remove providers that no longer practice, and ensure providers aren’t listed under the wrong type or with the wrong contact information. Improved directory accuracy for behavioral health providers will be beneficial for families using the directory, as well as for MHS schedulers who are part of the pilot program.
Although not part of the IG report, MOAA also recognizes that copay increases for mental health visits have created an additional barrier to access, particularly for retirees and their families. We are pursuing copay reductions for mental health outpatient visits to facilitate access to care.
MOAA Knows Why You Serve
We understand the needs and concerns of military families – and we’re here to help you meet life’s challenges along the way. Join MOAA now and get the support you need.